TMS for Treatment Resistant Depression – Achieving Remission is Possible
Treatment Resistant depression is depression that has not responded to 2-4 antidepressant medications and an adequate trial of evidence-based therapy (includes CBT, psychodynamic, and interpersonal therapy IPT). The mainstay of treatment for severe treatment resistant depression has been ECT for the past 50 plus years. TMS was developed in 1985 and approved by the FDA in 2008 for the first time and for Brainsway deepTMS in 2013. A recent article published in Psychiatric Times entitled TMS: A Useful Clinical Tool for Treatment-Resistant Depression by Abhijit Ramanujam, MD appeared in the December 2021 edition. In this article he summarizes how TMS works, when it is a good option, effectiveness, safety, and side effects. The following are some of the article’s highlights.
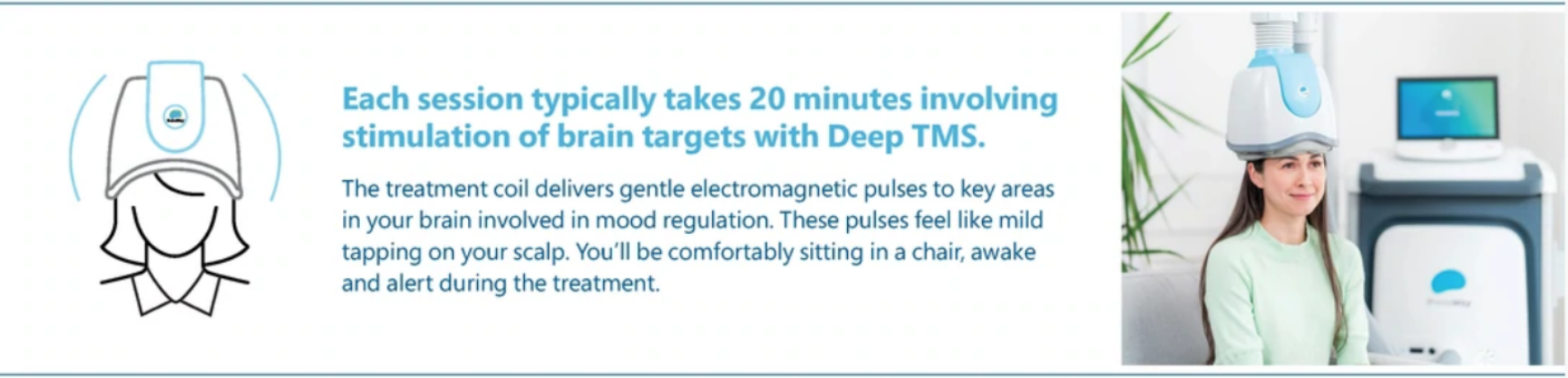
TMS uses alternating current passed through a coil of wires to generate a magnetic field. The magnetic field produces electric current which passes through the skull and stimulates a focal area of the brain. This stimulation is mild and is focused on the brain region specifically involved in depression. Functional imaging studies support this by showing TMS can change activity not only at the stimulation site but also distant sites connected functionally. Research has also shown that TMS has many molecular effects comparable to electroconvulsive therapy (ECT). Unlike ECT, TMS doesn’t require general anesthesia and does not cause cognitive impairment or memory loss and is done in an outpatient setting in a 30-minute appointment. Some other studies have shown normalized serotonin levels after TMS treatments and increased regional cerebral blood flow.
TMS is a good option for patients with unipolar depression who have failed 2-4 antidepressant trials and an adequate trial of evidence-based therapy. Patients are evaluated to confirm the primary diagnosis of treatment resistant depression and to rule out any contraindications. TMS is contraindicated in patients with: increased risks for seizures, implanted metallic hardware and unstable general medical disorders.
In trials for FDA approval, deepTMS was found to effectively reduce depressive symptoms by at least 50% in 75% of patients treated and to have a 50% remission rate. In these studies individuals were taken off their antidepressant medications, given TMS treatments (36 in a series) and then put on a maintenance mono medication to help prevent relapse. In clinical practice these rates of efficacy are higher as patients are encouraged to stay on antidepressants during TMS treatments.
TMS is generally well tolerated with very little side effects. The most serious potential side effect of TMS is a generalized tonic-clonic seizure. The risk of seizure is rare occurring in less than 0.1 to 0.5% of patients when safety guidelines are followed. The most common side effect reported is headache and scalp pain. In FDA studies for deep TMS the incidence of headache was the same in active verses placebo groups. Headache and scalp pain generally resolve over the first two weeks of treatment.
According to Dr. Ramanujam “TMS is an exciting and promising therapy that can provide real and lasting relief for patients with treatment-resistant depression. Conducted in an outpatient setting, TMS is a noninvasive procedure that is generally safe and well-tolerated.” If you would like to read the original article go to this websites home page and click on TMS and scroll down to the link for the Psychiatric Times article.